INTRODUCTION
Tobacco use is the leading cause of preventable deaths worldwide and is associated with increased risks of lung diseases, respiratory infections, and other communicable diseases1. COVID-19 poses additional risks to tobacco users, as they are considered more susceptible to exacerbated symptoms of COVID-192. The impaired lungs and weakened immune systems render smokers more vulnerable to the COVID-19 virus3. Moreover, our prior study suggests that smokers are more likely to contract COVID-19 because the virus may spread through frequent hand-to-mouth contact4. The evidence on e-cigarette (EC) use, though relatively limited, also suggests an increased risk of infection due to hand-to-mouth action, sharing of devices and the transmission of the virus in EC aerosols, and more severe outcomes due to the weakened respiratory system5.
Tobacco users respond differently to COVID-19. The pandemic might have led to reduced tobacco use or increased quit attempts due to raised health concerns among the public6-8 or by hindering access to cigarettes and social opportunities for smoking through COVID-related restrictions (such as lockdowns and reduced social gatherings)9. Conversely, increased tobacco use during the pandemic has also been reported in some countries (France, Iceland, USA and Brazil), potentially due to adverse psychosocial outcomes like anxiety and depression10-13, the need to relieve boredom during lockdowns and the perception of smoking as a coping mechanism for stress6. The COVID-19 outbreak in Hong Kong experienced two peaks in 2020, with the first peak on 9 February and a second wave in March. Sparing a city-wide lockdown, the Hong Kong Special Administrative Region government implemented stringent measures to contain the spread of the virus, including quarantine, social distancing, and school suspensions. Our previous study on adult tobacco users in Hong Kong found an 11.5% net decrease in overall tobacco use (cigarettes, ECs, HTPs) after the first two waves of the COVID-19 outbreak14.
Compared with the general population, young people are more susceptible to the adverse effects of social isolation15 and experience greater mental health problems16. They may engage more in risk-taking behaviors during the COVID-19 pandemic, partly due to their different risk perceptions17. A longitudinal study in the US of young adults found that lower perceived smoking risk predicted the initiation of cigarette use18. In US adolescents (aged 13–17 years), the perception that ‘EC use would increase one’s risk for contracting COVID-19’ was inversely correlated with past 30-day EC use19. However, the risk perception and changes in different tobacco products in adolescents during COVID-19 have not been reported.
While several quantitative studies have investigated changes in tobacco use due to COVID-19 in adolescents20,21, these studies rely on predetermined survey questions. They might not capture the complexity and variability of adolescents’ experiences in this context. Herein, we investigated the harm perceptions towards different tobacco products (cigarettes, ECs, and HTPs) and the impact of COVID-19 on behavioral changes in tobacco use among Hong Kong adolescent tobacco users.
METHODS
Adolescent tobacco users of cigarettes, ECs and HTPs were selected from the participants of the School-based Smoking Survey among Students in 2018–2019 (conducted before COVID-19) and 2020–2021 (conducted since the fourth wave of the COVID-19 outbreak in Hong Kong). The territory-wide crosssectional survey was conducted every two years among Hong Kong secondary school students (grades 2–6, typically aged 13–17 years). Students reported their tobacco use behaviors in detail and provided contact numbers for potential follow-up studies. An overview of the recruitment process is shown in Figure 1.
Eligible students were current users of any of the above three products before the outbreak of COVID-19 (December 2019 to January 2020) based on the question, ‘Before the outbreak of COVID-19, in December 2019, which of the following tobacco products were you using? (cigarettes, ECs or HTPs)’. From January to April 2021, we phoned all 736 tobacco users identified from the 2018–2019 round survey. Student tobacco users were also recruited by referral of existing participants. Data saturation was obtained from the first 13 cigarette users and 15 EC users. We identified more students who reported HTP use (n=160) with contact information in the 2020–2021 round survey and recruited eight current HTP users. Current cigarette users and EC users were also included in the analysis among those who reported ever HTP use in February 2022.
Telephone interviews were conducted using an interview guide (Supplementary file Part 1) covering two topics: 1) the perceived association of tobacco use with susceptibility to contracting COVID-19 and vulnerability to serious COVID-19 consequences by different tobacco products; and 2) the perceived impacts of the pandemic on tobacco use behaviors and changes in tobacco use since the outbreak of COVID-19. The experiences of tobacco use in both the early phase of the COVID-19 outbreak (February–March 2020) and later phases (July–August 2020 for Wave 3, November–December 2020 for Wave 4) were asked and collected, including changes in tobacco consumption, places of use, type of tobacco products and the underlying reasons. Interviews were conducted by three trained research staff. All interviewees provided verbal informed consent and were given incentives with a HK$100 (US$12.8) cash transfer or supermarket coupon after the interview. Ethics approval (No. UW 21-011) was granted by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster.
Analysis was led by two researchers, WL and CT. All interviews were audio-recorded and transcribed verbatim by four research assistants. The transcripts of each transcriber were randomly selected for accuracy checking. Data were prepared for analysis using NVivo qualitative software (version 12.0) (QSR International Pty. Ltd., 2012, Doncaster, Australia). Inductive coding and narrative analysis methods were adopted22 to construct the thematic framework and potential subthemes. Then, the transcripts and coded data were re-examined to build individual narratives and case histories. All transcripts were double-coded, with regular meetings held to review data by two researchers and a senior researcher. Disagreements were reconciled through discussion.
RESULTS
Participants and characteristics
Table 1 shows that of 40 participants, 63% (n=25) were boys, and 46% (n=18) were in Secondary school grade 6. Exclusive cigarette use was most common (n=15), followed by concurrent use of cigarettes and ECs (n=10), exclusive ECs use (n= 7), concurrent use of all three tobacco products (n=5), and concurrent use of ECs and HTPs (n=3). No one used HTPs exclusively. In total, 30 of them used cigarettes, 25 used ECs and 8 used HTPs.
Table 1
Demographic and tobacco-related characteristics of participants (N=40)
| Characteristics | n | %* |
|---|---|---|
| Sex | ||
| Boy | 25 | 63 |
| Girl | 15 | 38 |
| Age (years), mean ± SD | 14.5 ± 2.1a | |
| Grade | ||
| Secondary 2 | 4 | 10 |
| Secondary 3 | 9 | 23 |
| Secondary 4 | 2 | 5 |
| Secondary 5 | 7 | 18 |
| Secondary 6 | 18 | 45 |
| Tobacco use status before the outbreak of COVID-19 | ||
| Exclusive cigarette use | 15 | 38 |
| Concurrent use of cigarettes and ECs | 10 | 25 |
| Exclusive EC use | 7 | 18 |
| Concurrent use of ECs and HTPs | 3 | 8 |
| Concurrent use of cigarettes, ECs, and HTPs | 5 | 13 |
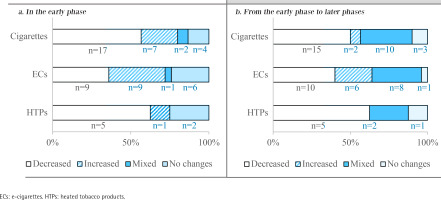
Figure 2 shows the major changes in tobacco use during the COVID-19 pandemic. Compared with the pre-pandemic phase, more cigarette users decreased their cigarette consumption than increased in both the early (17 vs 7) and later phases (15 vs 2) of COVID-19. An equal number of EC users decreased and increased their use in the early phase (9 vs 9), while more decreased than increased (10 vs 6) in later phases; 5 of 8 HTP users decreased their use in the early and later phases.
Figure 2
Changes in specific tobacco use in the early phase (Feb–Mar 2020) and later phases (July–Aug 2020, Nov–Dec 2020) of the COVID-19 pandemic
Additionally, 7 participants reported using new tobacco products during the pandemic: 3 cigarette users used ECs, 1 EC user used cigarettes, one dual user of cigarette and EC used HTPs, and two dual users of ECs and HTPs used waterpipe. Further details of changes in the tobacco use behaviors of all participants are shown in Supplementary file Table 1.
Perceived association between tobacco use and COVID-19
Participants held varying opinions on the relationship between tobacco use and COVID-19. Most participants considered tobacco users to be at a higher risk of contracting and would experience severe symptoms of COVID-19. According to the participants, this perception was influenced by several factors, including the potential for exposure to the virus when smoking without a mask, poor hand hygiene, worsened health outcomes and weakened immune systems associated with tobacco use.
Some participants, however, believed that tobacco users were at no greater risk of contracting COVID-19 or would not experience severe symptoms than non-tobacco users. They attributed the risk of contracting COVID-19 to personal hygiene practices and luck, and the severity of symptoms to general health. Additionally, one participant perceived a lower risk of infection or severity of COVID-19 associated with tobacco use due to the ‘protective function’ of substances in cigarettes.
Participants held conflicting views regarding the harmfulness of different tobacco products, with some perceiving ECs and HTPs as less harmful than traditional cigarettes, and EC/HTP users were at similar or lower risk of contracting COVID-19 or would experience less severe symptoms if infected.
Over half of the participants had limited knowledge (n=23) about the risks associated with EC/HTP use and COVID-19 and had limited access to reliable resources of information (n=22) on the association between tobacco use and COVID-19.
The most common sources of information of participants were ‘personal knowledge/experience’, ‘social media/online information’, ‘official news/TV’, and ‘friends’ experience’. Only a few participants (n=3) had ever learned about the association between tobacco use and COVID-19 from ‘schools or classrooms’. Further details of participants’ perceptions regarding the association between tobacco use and COVID-19 are shown in Supplementary file Table 2.
Table 2
Participants’ perceived impacts of COVID-19 and changes in tobacco use behaviors
Perceived COVID-19 impacts and changes in tobacco use behaviors: barriers and facilitators
According to participants’ responses, we found nine perceived impacts of the pandemic on tobacco use behaviors (Table 2). Of these, six were barriers to tobacco use, including COVID-19 policies, fear of COVID-19 infection, non-COVID-related health concerns, fewer social opportunities, financial issues, and limited access to tobacco products. Two factors were facilitators of tobacco use: the transition to online learning and negative emotions. The family/peer influence on individuals’ tobacco use behaviors during the epidemic had both positive and negative effects. Changes were found in tobacco consumption, smoking places and the type of tobacco products used. Additional information on COVID-19 impacts and changes in tobacco use is available in Supplementary file Table 3.
Barriers
The COVID-19 policies were a common factor that influenced adolescent tobacco use. Participants had shifted tobacco use from outside to mainly at home or inconspicuous public places as masking was mandatory by law with no exemption for smoking.
Many participants reduced or quit tobacco use in response to COVID-19 policies, which restricted smoking outside through measures such as mandatory masking regulations and high fines (HK$5000). The prolonged period spent at home due to social distancing restrictions and school closures also contributed to this change, particularly since many participants lived with their families and were unable to smoke at home due to disapproval from family members.
Another barrier to adolescent tobacco use is the fear of COVID-19 infection, which has reduced or quit tobacco use in some participants. They reported concerns about the heightened risk of infection associated with smoking due to the need to remove masks in public places and inhale deeply.
In addition to the direct impact of COVID-19, the pandemic has heightened the concerns of adolescents about their health and led to decreased tobacco use in many. Some adolescents also experienced health problems or perceived their situation as worsening during the pandemic, which further prompted them to decrease tobacco use.
Many participants reduced their cigarette use due to the limited social interaction opportunities caused by social isolation. To reduce smoking, several participants actively reduced socializing with smoking friends, and one even ‘cut off contact with smoking friends’.
Several participants decreased tobacco use or switched to other tobacco products due to the difficulty of access to tobacco products and financial concerns amid the pandemic. A few participants reported no change in tobacco consumption as they still had access to tobacco products online without age limit restrictions:
‘I bought ECs online, such as from IG shops, because you don't need to provide an ID card for age verification.’ (No. 35, Girl, S2, ECs and HTPs)
Facilitators
Participants reported that the transition to online learning led to increased tobacco use due to a lack of supervision and boredom.
Several participants expressed that the transition to online learning led them to smoke more because they had difficulty focusing on schoolwork and could not follow a structured schedule or prepare for exams in the same way as they would in a physical classroom.
Negative emotions, such as stress, anxiety and loneliness during the pandemic, was a factor in increased tobacco use. Participants expressed that smoking helped them to relieve stress and anxiety, and to pass the time during periods of social isolation.
Mixed impacts and other changes
The impact of family/peer influence during the pandemic was mixed. Some participants reported reducing tobacco use due to discouragement from their family or peer group. Others, however, reported that their peer group either introduced them to new tobacco products or activities provided tobacco products to them, leading to trying new tobacco products.
EC use was less affected than cigarette/HTP use during the pandemic. Some participants found ECs more convenient to use indoors or outside while wearing a mask as it produces less smoke and odor. Even though the long time spent at home restricted the cigarette use of some participants, the reduced cigarette use was compensated by increased EC use in some participants.
Some participants reported increased tobacco consumption in later phases of COVID-19 due to the ‘anti-pandemic fatigue’. As they grew accustomed to the ongoing pandemic and COVID-19 restrictions, they resumed smoking despite the health risks.
DISCUSSION
This is a novel qualitative study investigating adolescents’ harm perception towards tobacco use and changes in tobacco use in the pandemic. The results showed that adolescents had limited knowledge of the risk of COVID-19 from tobacco use, particularly from EC/HTP use. Their risk perception of tobacco use in relation to COVID-19 was based on personal experiences or observations of friends rather than from WHO, government departments or other authoritative or credible sources. More adolescents had decreased than increased tobacco consumption while others showed a mixed pattern of changes with decreases and increases. EC use was the least affected. A few tobacco users had initiated the use of other products, including ECs/HTPs and waterpipe. Some switched from cigarettes to ECs or HTPs or both, and from smoking outside to smoking mainly at home or in hidden places outside. We found more barriers than facilitators of tobacco use, but family/peer influence had mixed impacts.
Our results are consistent with a qualitative study that reported much confusion in US young adults on the association between tobacco use and COVID-19, especially for EC use compared with cigarette use23. Results on the association between COVID-19 and tobacco use, particularly ECs and HTPs during the early stage of the pandemic were scarce in the literature, and in reports and messages in mass and social media. The limited knowledge and sources of reliable information, and hence such perception and confusion, are not unexpected in our adolescents, and in young adults and adults elsewhere. Such results could reflect the failure of timely and effective communication to the whole population in many countries to use the facts about the known harms of tobacco use to promote tobacco control amid the pandemic. As more results on the associations between COVID-19 and various tobacco products are emerging, the opportunities to use such results for tobacco control should not be missed again.
We found both increases and decreases in tobacco use among adolescents, but more adolescents had decreased tobacco use than increased. This finding is consistent with cross-sectional studies in Turkish24 and Indonesian adolescents25, which reported greater decreases than increases in adolescent tobacco use amid the COVID-19 pandemic. But these studies did not investigate differences in changes in different tobacco products. Our qualitative study addressed this gap in adolescents and found that EC use was less affected than cigarette/HTP use amid the pandemic. Some participants even reported increased consumption of ECs or switching from cigarettes/HTPs to ECs when smoking at home. This aligns with a study in US young people that reported an increase in EC use due to changes in daily environment that made EC use a more feasible option26. Adolescents would feel that they could use them more freely than cigarettes in places where conventional cigarettes or HTPs would be more easily detected, such as in their homes or at school27. Notably, we found easy access to cigarettes or ECs in adolescents, despite that sales to minors are prohibited. In contrast to a previous study in US youth and young adults that reported barriers to EC access due to COVID-19 policies28, only one adolescent in our study reported difficulty in buying EC pods. In Hong Kong, even though the manufacture, import, advertising, distribution, and sale of ECs and HTPs have been banned since 30 April 2022, the use and non-commercial possession of such products are not prohibited. Whether the new regulations have been successful in minimizing adolescent use of such products is uncertain. These findings are warning and suggest an urgent need for strong enforcement of the regulations and monitoring of the impacts on adolescent tobacco use in Hong Kong.
We found more barriers than facilitators to tobacco use in adolescents amid COVID-19. COVID-19 policies, especially masking mandates and social gathering restrictions, have served as a deterrent, resulting in reduced tobacco consumption and smoking outside in our study. Some adolescents changed from smoking openly to secluded places such as small alleys or turning to ‘fast smoking’ to avoid the heavy fines and reduce the risk of infection from unmasking and smoking. The deterring effect was great, as this fine (HK$5000, US$1=HK$7.8) is much greater than that of HK$1500 for smoking in places where smoking is prohibited. These behaviors were also observed in US young adults23, US adults29 and Hong Kong adults30. After Hong Kong lifted the mandatory mask-wearing requirement on 1 March 202331, concerns about an increase in smoking prevalence after opening up have been raised by the government, tobacco control advocates and in the mass media.
Our study found that spending more time at home due to social gathering restrictions and fewer social opportunities decreased adolescent tobacco use, which is consistent with previous studies on US college students32 and adolescents21. Importantly, our findings found that ‘anti-pandemic fatigue’ during later phases of the COVID-19 pandemic led some participants to resume increased tobacco use, resulting in mixed changes in adolescent smoking behavior. These findings suggest that the pandemic might have only temporarily deterred tobacco use in adolescents. As we approach the end of the COVID-19 pandemic, further studies are necessary to assess the long-term impact of the pandemic on tobacco use in adolescents.
The other barriers to adolescent tobacco use in our study included financial problems, limited access to tobacco products, fear of COVID-19 infection and non-COVID-related health concerns. These factors discouraged tobacco use in many adolescents but not all. In our study, financial problems generally led to decreased smoking frequency and consumption. These findings support that raising the tobacco tax is an effective strategy for deterring young people from using tobacco products, especially for those not financially well off. Although the pandemic did not directly affect the availability of cigarettes in retail stores, as Hong Kong had no lockdown, many adolescents reported going out less often due to fear of infection. While such fear was not the most commonly reported influential factor, young smokers generally perceived themselves to be at a lower risk of COVID-19 infection and its health consequences compared to adult smokers33. Whether emphasis on the risks of COVID-19 and increasing fear would motivate more adolescents to quit smoking is uncertain.
Our study found greater freedom at home and negative emotions as major facilitators of tobacco use among adolescents. In Hong Kong, as in other regions with school closures, the shift to online learning during the pandemic might have contributed to increased EC use. Students had more time to stay at home and less supervised time than in schools where smoking is not permitted, especially when they are alone at home. Furthermore, negative emotions associated with the pandemic, such as boredom or academic pressure, could have further exacerbated these facilitators of smoking. A survey study on Canadian adolescents showed that tobacco use was an avoidant stress-coping strategy in the early phase of the pandemic34,35. The sudden shift to remote learning presented great challenges for adolescents, with some having difficulty transitioning to virtual learning amid the pandemic36. Finally, the results of more barriers than facilitators of tobacco use corroborated the results of more adolescents decreased than increased tobacco use. As the pandemic is nearing its end and the barriers associated with COVID-19 are diminishing, our results support the worry of increased tobacco use after the relaxation of all control measures and the opening up in Hong Kong and elsewhere. Further studies and monitoring on the effects of opening up on tobacco and nicotine product use in adolescents (as well as in adults) are needed to inform policies.
Limitations
Our study has some limitations. First, tobacco use status was self-reported without validation by biochemical tests. Second, the number of HTP users was small as their use was less common than that of ECs and cigarettes. Third, whether our results could be generalized to other places with different COVID-19 control measures and smoking prevalence is uncertain. Additionally, the qualitative design of our study did not allow for statistical inference, so the findings should be interpreted with caution. Lastly, it is important to note that the results might not be applicable to different age groups, as our focus was on adolescents in Hong Kong.
CONCLUSIONS
Adolescents had limited sources of reliable information on COVID-19 risks from tobacco use, especially from ECs and HTPs. While more adolescents had decreased than increased tobacco consumption during the pandemic, EC use was the least affected. Tobacco use had shifted from outside to mainly at home or hidden areas. COVID-19 and related social changes may both facilitate or deter adolescent tobacco use. The insights gained from our study can inform ongoing research to reduce tobacco use and future policy development to respond to crises such as COVID-19. Even though the pandemic is fading, closely monitoring the long-term impact of tobacco use remains necessary.



