INTRODUCTION
Secondhand smoke exposure (SHSE) increases risks to many diseases, such as cardiovascular diseases and cancers in adults, and respiratory diseases and poor mental health outcomes in both children and adults1. Globally, SHSE causes an estimated 0.88 million deaths, of which 75% are non-smokers2. Hence, combating SHSE, particularly in workplaces and public spaces, is a key component of worldwide tobacco control policies. The World Health Organization (WHO) Framework Convention on Tobacco Control (FCTC) requires member states to enact comprehensive measures that protect the general population from SHSE at work (SHSEwork) and public spaces3, such as legislating smoking bans in indoor workplaces, indoor public places, and public transport. This is necessary as workplaces without smoking restrictions increase the risk to SHSE, with some workplaces constituting higher risk than others4,5. Previous studies have reported that some groups of workers, such as males, ethnic minorities, younger workers, and those with lower education level4,5 have greater odds of SHSEwork.
FCTC campaigns actively advocate for the adoption of smoke-free homes, as research shows children are at greater risk to SHSE than adults6, and more than 40% of youths globally are exposed to secondhand smoke (SHS) at home and have parents who smoke at home7. Risk of SHSE increases among children living with a smoker, and they have poorer health outcomes both during childhood and in the future as adults1. In particular, children living with a father or sibling who smoked at home is associated with earlier and/or greater odds of smoking initiation and having positive attitudes towards smoking and other tobacco-related health outcomes8,9. This suggests childhood SHSE and identity of the smoker at home may play a role in other future tobacco-related situations and outcomes, such as willingness to be exposed to SHS at work in adulthood. In addition, studies have shown that among people who are exposed to SHS at home, a vast majority are also exposed to SHS at work10. Overtime, SHSE at home (SHSEhome) and at work (SHSEwork) have decreased in tandem11. This suggests an association between SHSE at different physical settings.
To the best of our knowledge, the relationship between SHSE in different temporal and physical settings, especially within multi-ethnic Asian populations, are not fully understood. Singapore is a highly urbanized city-state in Asia with strict tobacco regulations, and had managed to lower smoking prevalence from almost 25% in the 1970s12 to 10% today13. Simultaneously, there is evidence that public perception and attitudes towards smoking has become less positive14, suggesting a shift towards social norms more hostile towards tobacco use, which is also observed in other developed economies15,16. As other Asian societies also become increasingly urban and cosmopolitan, Singapore’s multi-ethnic population provides an opportunity for this investigation. Studies from Western countries may be limited, given the need to contextualize the impact of culture and social norms on tobacco-related outcomes and behaviors in different societies17. We investigate the associations of childhood (age ≤18 years) and current SHSEhome with current SHSEwork, among healthy adults who are never smokers, in Singapore, and whether these associations could be further explained by the sources of daily smokers at home.
METHODS
Study population
This cross-sectional study used information collected from Phase 1 of the Singapore Multi-Ethnic Cohort18 (MEC), a population-based study (see link for detailed information on the cohort: https://blog.nus.edu.sg/sphs/population-studies/multi-ethnic-cohort-phase-1-mec1/). In brief, recruitment of adults (age ≥21 years) from the three major ethnic groups (i.e. Chinese, Malay, Indian) in Singapore was conducted between 2004 and 2010, mainly from other existing cohort studies. Ethics approval for this sub-study was obtained from the Department Ethics Review Committee in Saw Swee Hock School of Public Health at National University of Singapore (SSHSPH-022).
Only never smoking, healthy and employed participants were included in this study. Participants were considered healthy if they responded ‘no’ to a series of questions regarding pre-existing chronic conditions in the survey (i.e. heart disease, stroke, high blood pressure, diabetes, high cholesterol, asthma, cancer, rheumatism, mental illness and other). Participants with missing information on any outcome, exposure and covariate variables were excluded from the analysis.
Variables used in analysis
Outcome
SHSEwork was coded as 1 (or 0) when the response was ‘yes’ (or ‘no’) to the question: ‘Are you currently exposed to cigarette smoke at work on a daily basis?’.
Exposures
Childhood SHSEhome were coded as 1 (or 0) when the response was ‘yes’ (or ‘no’) to the questions: ‘From your birth to age 18 years, did anyone living in your home smoke at home on a daily basis for 6 months or longer?’ and ‘Does anyone who currently stays with you smoke on a daily basis?’. SHSEhome exposure characteristics in terms of sources of persons who smoked daily at home were available for selection by participants if they responded ‘yes’ to the previous questions. For childhood SHSEhome, five exposure sources were available: 1) father, 2) mother, 3) sibling, 4) grandparent, and 5) other. For current SHSEhome, responses were coded as 1 (or 0) when the response was ‘yes’ (or ‘no’) to the question: ‘Does anyone who currently stays with you smoke on a daily basis?’. Four exposure sources were identified: 1) spouse, 2) child, 3) parent/in-law, and 4) other. For each identity, a binary variable was generated indicating whether the response by the participant was ‘yes’.
Covariates
Covariates for the multiple logistic regression model were grouped into three broad categories: sociodemographics (age, gender, ethnicity, education level, marital status, and type of residence), lifestyle (ever drank alcohol, weekly physical activity level, and daily consumption of fresh fruits, vegetables, dairy products, poultry, red meat and seafood) and current health status proxied by clinical measurements [body mass index (BMI), mean arterial pressure (MAP), triglyceride level (TG), low-density lipoprotein cholesterol level (LDL), high-density lipoprotein cholesterol level (HDL) and hemoglobin A1c (HbA1c)]. All continuous variables were categorized into quartiles, except BMI which was categorized into four categories according to WHO’s recommendation for Asia-Pacific populations. These variables were chosen as they have been shown to be associated with tobacco-related health outcomes, including SHSE19,20.
Statistical analysis
All analyses were conducted using R version 4.0.2. Frequencies and percentages were used to summarize categorical variables representing participants’ characteristics. Fisher’s exact test was used to assess the association between categorical variables and SHSEwork.
A parsimonious multiple logistic regression model was developed using the forward stepwise approach to obtain adjusted odds ratios (AORs) of childhood and current SHSEhome on current SHSEwork (Model 1). All covariates were available for selection into the final model during the model building process while the variables in a base model, which included both temporal settings of SHSEhome, were not allowed to exit during model building process. Covariates entered or exited at each step of the model building process based on whether they improved the model fit by utilizing the Akaike Information Criterion (AIC). Thereafter, Model 1 was the base model in the forward stepwise approach when investigating whether the associations of childhood and current SHSEhome with SHSEwork could be further explained by the sources of daily smokers at home (Model 2). All identity-related variables (i.e. all binary variables related to sources of daily smokers) were available for selection into the final model during the model building process (i.e. forward stepwise approach). Interaction between the childhood and current SHSEhome were assessed to determine whether the two effects of SHSEhome were independent. If these effects were not independent, all identity-related variables in Model 2 had their two-way interactions assessed regardless whether they were sources from childhood or current. Otherwise, identity-related variables from the same temporal setting in Model 2 had their two-way interactions assessed where applicable. For each AOR that was attributable to participants from the same SHSEhome profile (e.g. experienced childhood SHSEhome and lived with father and sibling(s) who smoked daily at home during childhood), it was decomposed into AORs that corresponded to SHSEhome characteristics (i.e. childhood and current SHSEhome, and identity-related variables) in Model 2. To corroborate the computed AORs of subgroups, the categorical variable representing the subgroups would be included as a predictor in the model and adjusted for the same covariates as Model 2 (Model 3). See the Supplementary file for further elaboration on this decomposition.
RESULTS
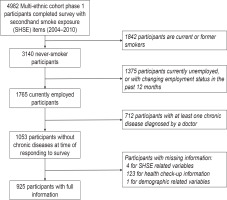
Figure 1 is the flow chart of participants’ selection that included 925 never smokers, employed, and healthy participants with complete information used in this analysis. Table 1 presents the characteristics of the participants. Overall, the majority of participants were female (66.8%), of Chinese ethnicity (45.3%), had pre-university education (37.0%), lived in HDB 4-room flats (40.3%), and were married (68.1%). The average age of participants was 38.7 years (SD=10.5). In total, 144 (15.6%) were exposed to SHS at work, while 217 (23.5%) were currently exposed to SHS at home; and among them the two most common sources of SHSEhome were the spouse (47.5%) and parent/in-law (28.1%). Similarly, 483 participants (52.2%) were exposed to daily SHSEhome during childhood. Among those respondents, the two most common sources of exposure were the father (86.7%) and siblings (21.9%). Having at least one sibling who smoked daily at home during childhood was significantly associated with current SHSEwork. For current SHSEhome, having at least one parent or parent in-law and at least one other source who smoked daily at home was significantly associated with reporting current SHSEwork. Participants who were younger, males, Indians, with pre-university education, never married, those who reported a lower consumption of fresh fruits, lower HDL and lower HbA1c, were more likely to report current SHSEwork.
Table 1
Characteristics of participants (N=925)
| Characteristics of SHSE at home (SHSEhome) | Current SHSE at work (SHSEwork) on a daily basis | |||
|---|---|---|---|---|
| Total (N=925) | Yes (N=144; 15.6%) | No (N=781; 84.4%) | pa | |
| n (%) | n (%) | n (%) | ||
| SHSEhome on a daily basis | ||||
| Temporal setting: Childhood (age ≤18 years) | 0.084 | |||
| No | 442 (47.8) | 59 (13.3) | 383 (86.7) | |
| Yes | 483 (52.2) | 85 (17.6) | 398 (82.4) | |
| Temporal setting: Current | 0.001 | |||
| No | 708 (76.5) | 94 (13.3) | 614 (86.7) | |
| Yes | 217 (23.5) | 50 (23.0) | 167 (77.0) | |
| Identities of daily smokers at home | ||||
| Temporal setting: Childhood (age ≤18 years) | ||||
| Father | 419 (45.3) | 76 (18.1) | 343 (81.9) | 0.056 |
| Mother | 21 (2.3) | 2 (9.5) | 19 (90.5) | 0.759 |
| Sibling | 106 (11.5) | 26 (24.5) | 80 (75.5) | 0.010 |
| Grandparent | 16 (1.7) | 2 (12.5) | 14 (87.5) | 1.000 |
| Other | 19 (2.1) | 3 (15.8) | 16 (84.2) | 1.000 |
| Temporal setting: Current | ||||
| Spouse | 103 (11.1) | 15 (14.6) | 88 (85.4) | 0.886 |
| Child | 27 (2.9) | 8 (29.6) | 19 (70.4) | 0.055 |
| Parent/in-law | 61 (6.6) | 17 (27.9) | 44 (72.1) | 0.010 |
| Other | 51 (5.5) | 16 (31.4) | 35 (68.6) | 0.004 |
| Sociodemographics | ||||
| Age (years) | <0.001 | |||
| Q1: <30 | 216 (23.4) | 54 (25.0) | 162 (75.0) | |
| Q2: 30 to <39 | 236 (25.5) | 37 (15.7) | 199 (84.3) | |
| Q3: 39 to <46 | 225 (24.3) | 28 (12.4) | 197 (87.6) | |
| Q4: ≥46 | 248 (26.8) | 25 (10.1) | 223 (89.9) | |
| Gender | <0.001 | |||
| Female | 618 (66.8) | 58 (9.4) | 560 (90.6) | |
| Male | 307 (33.2) | 86 (28.0) | 221 (72.0) | |
| Ethnicity | 0.001 | |||
| Chinese | 419 (45.3) | 45 (10.7) | 374 (89.3) | |
| Malay | 222 (24.0) | 42 (18.9) | 180 (81.1) | |
| Indian | 284 (30.7) | 57 (20.1) | 227 (79.9) | |
| Education level | <0.001 | |||
| Primary and lower | 157 (17.0) | 19 (12.1) | 138 (87.9) | |
| Secondary | 251 (27.1) | 28 (11.2) | 223 (88.8) | |
| Pre-university | 342 (37.0) | 79 (23.1) | 263 (76.9) | |
| University and higher | 175 (18.9) | 18 (10.3) | 157 (89.7) | |
| Housing typeb | 0.481 | |||
| HDB 1–2 rooms | 26 (2.8) | 4 (15.4) | 22 (84.6) | |
| HDB 3 rooms | 177 (19.1) | 34 (19.2) | 143 (80.8) | |
| HDB 4 rooms | 373 (40.3) | 57 (15.3) | 316 (84.7) | |
| HDB 5 rooms/executive flat/condo/landed/other | 349 (37.7) | 49 (14.0) | 300 (86.0) | |
| Marital status | 0.007 | |||
| Married | 630 (68.1) | 82 (13.0) | 548 (87.0) | |
| Never married | 245 (26.5) | 52 (21.2) | 193 (78.8) | |
| Widowed/divorced/separated | 50 (5.4) | 10 (20.0) | 40 (80.0) | |
| Consumption habits | ||||
| Alcoholic drink | 0.103 | |||
| No | 461 (49.8) | 81 (17.6) | 380 (82.4) | |
| Yes | 464 (50.2) | 63 (13.6) | 401 (86.4) | |
| Fresh fruits (g/day) | <0.001 | |||
| Q1: <100.8 | 231 (25.0) | 41 (17.7) | 190 (82.3) | |
| Q2: 100.8 to <188.0 | 232 (25.1) | 51 (22.0) | 181 (78.0) | |
| Q3: 188.0 to <303.8 | 230 (24.9) | 18 (7.8) | 212 (92.2) | |
| Q4: ≥303.8 | 232 (25.1) | 34 (14.7) | 198 (85.3) | |
| Vegetables (g/day) | 0.129 | |||
| Q1: <100.2 | 231 (25.0) | 30 (13.0) | 201 (87.0) | |
| Q2: 100.2 to <152.4 | 231 (25.0) | 42 (18.2) | 189 (81.8) | |
| Q3: 152.4 to <220.1 | 231 (25.0) | 43 (18.6) | 188 (81.4) | |
| Q4: ≥220.1 | 232 (25.1) | 29 (12.5) | 203 (87.5) | |
| Dairy products (g/day) | 0.241 | |||
| Q1: <75.9 | 232 (25.1) | 27 (11.6) | 205 (88.4) | |
| Q2: 75.9 to <151.3 | 231 (25.0) | 40 (17.3) | 191 (82.7) | |
| Q3: 151.3 to <287.1 | 230 (24.9) | 36 (15.7) | 194 (84.3) | |
| Q4: ≥287.1 | 232 (25.1) | 41 (17.7) | 191 (82.3) | |
| Poultry (g/day) | 0.244 | |||
| Q1: <23.0 | 232 (25.1) | 30 (12.9) | 202 (87.1) | |
| Q2: 23.0 to <40.8 | 231 (25.0) | 40 (17.3) | 191 (82.7) | |
| Q3: 40.8 to <70.5 | 231 (25.0) | 31 (13.4) | 200 (86.6) | |
| Q4: ≥70.5 | 231 (25.0) | 43 (18.6) | 188 (81.4) | |
| Red meat (g/day) | 0.350 | |||
| Q1: <11.6 | 231 (25.0) | 35 (15.2) | 196 (84.8) | |
| Q2: 11.6 to <24.1 | 231 (25.0) | 44 (19.0) | 187 (81.0) | |
| Q3: 24.1 to <53.6 | 231 (25.0) | 30 (13.0) | 201 (87.0) | |
| Q4: ≥53.6 | 232 (25.1) | 35 (15.1) | 197 (84.9) | |
| Seafood (g/day) | 0.819 | |||
| Q1: <32.5 | 231 (25.0) | 37 (16.0) | 194 (84.0) | |
| Q2: 32.5 to <55.2 | 231 (25.0) | 36 (15.6) | 195 (84.4) | |
| Q3: 55.2 to <83.8 | 231 (25.0) | 39 (16.9) | 192 (83.1) | |
| Q4: ≥83.8 | 232 (25.1) | 32 (13.8) | 200 (86.2) | |
| Weekly physical activity level (met-hr/week) | 0.215 | |||
| Q1: <63.5 | 231 (25.0) | 35 (15.2) | 196 (84.8) | |
| Q2: 63.5 to <99.8 | 231 (25.0) | 27 (11.7) | 204 (88.3) | |
| Q3: 99.8 to <136.6 | 231 (25.0) | 40 (17.3) | 191 (82.7) | |
| Q4: ≥136.6 | 232 (25.1) | 42 (18.1) | 190 (81.9) | |
| Current health status | ||||
| Body mass index (kg/m2) | 0.417 | |||
| Underweight: <18.5 | 42 (4.5) | 3 (7.1) | 39 (92.9) | |
| Normal: 18.5 to <23.0 | 332 (35.9) | 50 (15.1) | 282 (84.9) | |
| Overweight: 23.0 to <27.5 | 314 (33.9) | 50 (15.9) | 264 (84.1) | |
| Obese: ≥27.5 | 237 (25.6) | 41 (17.3) | 196 (82.7) | |
| Triglyceride level (mmol/L) | 0.991 | |||
| Q1: <0.62 | 222 (24.0) | 34 (15.3) | 188 (84.7) | |
| Q2: 0.62 to <0.87 | 239 (25.8) | 36 (15.1) | 203 (84.9) | |
| Q3: 0.87 to <1.30 | 231 (25.0) | 37 (16.0) | 194 (84.0) | |
| Q4: ≥1.30 | 233 (25.2) | 37 (15.9) | 196 (84.1) | |
| Low-density lipoproteins (mmol/L) | 0.068 | |||
| Q1: <2.72 | 229 (24.8) | 31 (13.5) | 198 (86.5) | |
| Q2: 2.72 to <3.25 | 232 (25.1) | 27 (11.6) | 205 (88.4) | |
| Q3: 3.25 to <3.87 | 232 (25.1) | 46 (19.8) | 186 (80.2) | |
| Q4: ≥3.87 | 232 (25.1) | 40 (17.2) | 192 (82.8) | |
| High-density lipoproteins (mmol/L) | <0.001 | |||
| Q1: <1.00 | 221 (23.9) | 46 (20.8) | 175 (79.2) | |
| Q2: 1.00 to <1.24 | 236 (25.5) | 41 (17.4) | 195 (82.6) | |
| Q3: 1.24 to <1.48 | 229 (24.8) | 39 (17.0) | 190 (83) | |
| Q4: ≥1.48 | 239 (25.8) | 18 (7.5) | 221 (92.5) | |
| Hemoglobin A1c (%) | 0.009 | |||
| Q1: <5.5 | 205 (22.2) | 39 (19.0) | 166 (81.0) | |
| Q2: 5.5 to <5.7 | 223 (24.1) | 46 (20.6) | 177 (79.4) | |
| Q3: 5.7 to <5.9 | 241 (26.1) | 27 (11.2) | 214 (88.8) | |
| Q4: ≥5.9 | 256 (27.7) | 32 (12.5) | 224 (87.5) | |
| Mean arterial pressure (mmHg) | 0.141 | |||
| Q1: <75.3 | 230 (24.9) | 30 (13.0) | 200 (87.0) | |
| Q2: 75.3 to <82.3 | 218 (23.6) | 39 (17.9) | 179 (82.1) | |
| Q3: 82.3 to <90.3 | 244 (26.4) | 31 (12.7) | 213 (87.3) | |
| Q4: ≥90.3 | 233 (25.2) | 44 (18.9) | 189 (81.1) | |
Figure 2 presents the associations between characteristics of SHSEhome and current SHSEwork, after adjusting for the covariates that enter the model through model building (i.e. age, gender, education level, ethnicity, marital status, ever consumed an alcohol beverage, consumption levels of fruits, and HbA1c levels). Association for childhood SHSEhome (Model 1: AOR=1.43; 95% CI: 0.93–2.19) and current SHSEhome (Model 1: AOR=2.05; 95% CI: 1.28–3.29) with current SHSEwork were both positive, but only the latter was statistically significant. When sources of daily smokers at home were entered into Model 1 through model building, the association for childhood SHSEhome remained non-significant (Model 2: AOR=0.54; 95% CI: 0.20–1.44) while the association for current SHSEhome (Model 2: AOR=1.78; 95% CI: 1.08–2.95) remained significant and positive.
Figure 2
Associations between characteristics of secondhand smoke exposure (SHSE) at home (SHSEhome) and current SHSE at work (SHSEwork)
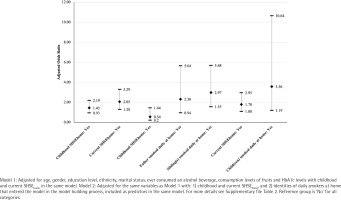
Two out of the five sources of exposure to SHS during childhood were then entered into the model (i.e. father and sibling). Specifically, living with a father (Model 2: AOR=2.30; 95% CI: 0.94–5.64) and at least one sibling (Model 2: AOR=2.97; 95% CI: 1.55–5.68) who smoked daily at home during childhood was positively associated with current SHSEwork, where the latter was significant. Only one out of the four sources from current enter the model (i.e. child). Specifically, living with at least one child who currently smokes daily at home was associated with current SHSEwork (Model 2: AOR=3.56; 95% CI: 1.19–10.64). We did not find a significant interaction between childhood and current SHSEhome in Model 1 (p=0.914) and Model 2 (p=0.755). Similarly, interactions between the two sources of exposure from childhood that enter the model were not significant (p=0.626).
Based on the sources that enter Model 2, we classified participants into subgroups that contain SHSEhome profiles with the same adjusted odds ratio. Since the interaction analyses suggest the associations of childhood and current SHSEhome are independent, Table 2 presents the AORs of subgroups at each temporal setting with the reference subgroup corresponding to no SHSEhome in the same temporal setting. The AOR between the subgroup with no childhood SHSEhome and each of the subgroups experiencing childhood SHSEhome were not significantly different except for the subgroup with combinations of SHS sources that include both father and sibling as daily smokers at home (Model 2: AOR=3.70; 95% CI: 1.88–7.30). This subgroup contains combinations, such as father and sibling only, and father and sibling with one or more of the following three sources of exposure: mother, grandparent, and other.
Table 2
Associations between subgroups of secondhand smoke exposure (SHSE) at home (SHSEhome) profiles and current SHSE at work (SHSEwork)
| Subgroups of SHSEhome profiles on a daily basis | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|
| n (%) | AOR | 95% CI | p | AOR | 95% CI | p | |
| Temporal setting: Childhood (age ≤18 years) | |||||||
| No childhood SHSEhome (Ref.) | 442 (47.8) | 1 | 1 | ||||
| Experienced childhood SHSEhome and combinations of identitiesa | |||||||
| Excluded father and siblingb | 28 (3.0) | 0.54 | 0.20–1.44 | 0.220 | 0.70 | 0.18–2.81 | 0.618 |
| Included father but excluded siblingc | 349 (37.7) | 1.25 | 0.78–1.99 | 0.348 | 1.23 | 0.77–1.97 | 0.383 |
| Excluded father but included siblingd | 36 (3.9) | 1.61 | 0.65–3.97 | 0.301 | 1.42 | 0.50–4.06 | 0.511 |
| Included both father and siblinge | 70 (7.6) | 3.70 | 1.88–7.30 | <0.001 | 3.90 | 1.92–7.89 | <0.001 |
| Temporal setting: Current | |||||||
| No current SHSEhome (Ref.) | 708 (76.5) | 1 | 1 | ||||
| Experienced current SHSEhome and combinations of identitiesa | |||||||
| Excluded childf | 190 (20.5) | 1.78 | 1.08–2.95 | 0.024 | 1.78 | 1.07–2.94 | 0.025 |
| Included childg | 27 (2.9) | 6.35 | 2.19–18.40 | 0.001 | 6.43 | 2.21–18.67 | 0.001 |
AOR: adjusted odds ratio. Model 2: Obtained AORs of subgroups by multiplying relevant AORs of SHSEhome characteristics from Model 2 (see Table 2). Model 3: Included two categorical variables representing the subgroups of childhood and current SHSEhome profiles as predictors in the model with adjustment for the same covariates as Model 2 (see footnotes in Table 2 for details of covariates).
For current SHSEhome, the subgroup experiencing current SHSEhome with combinations of sources that exclude children as the current daily smoker at home (i.e. combinations with one or more of these three sources: spouse, parent/in-law, and other) had significantly higher odds of reporting exposure than the subgroup with no current SHSEhome (Model 2: AOR=1.78; 95% CI: 1.08–2.95). When the combinations of sources include also children in the home, the odds further increased (Model 2: AOR=6.35; 95% CI: 2.19–18.40). Similar results were obtained when we represented these subgroups of SHSEhome profiles from two temporal settings as two categorical variables and include them as predictors into one model with adjustment for the same covariates as Model 2 (Model 3).
DISCUSSION
We investigate associations of childhood SHSEhome and current SHSEhome with current SHSEwork, among healthy and employed adults who were never smokers, in Singapore. Although it is only the association between current SHSEhome and SHSEwork that is significant and positive, the associations of childhood and current SHSEhome with SHSEwork are further explained by the sources of daily smokers at home. For childhood SHSEhome, the two sources were the father and siblings. Although both sources increase the odds of current SHSEwork, only exposure via siblings was significant. However, when compared to no childhood SHSEhome, the odds were only significantly higher among exposed participants who lived with their fathers and siblings who smoked daily at home during their childhood. For current SHSEhome, regardless of the identity of daily smokers at home, the odds among the exposed is significantly higher than the odds among the unexposed. But participants living with their children who are current daily smokers at home led to significantly elevated odds.
Our results highlight the need to consider sources of smokers at home to gain deeper insights into the impact of SHSEhome on current SHSEwork, indicating the importance of familial relationships and dynamics. Considering only the occurrence of SHSE without factoring in the other underlying characteristics of SHSE could prematurely lead to false negative findings for childhood SHSEhome. Existing studies found social relationships are closely linked with tobacco use in general21, and hence could potentially be linked with other tobacco-related issues, such as SHSE in different physical settings and throughout one’s life-course. Parents’, siblings’ and peers’ attitudes and behaviors play significant roles in shaping children’s and adolescents’ attitudes towards tobacco smoking8,9, and evidence supports that the roles played by these different social relations are independent. Similarly, our results suggest that although living with either father or sibling who smoked increase the odds of current SHSEwork independently, it is the sibling identity that may play a greater role.
When the sources of childhood daily smokers at home include both father and sibling, the odds of current SHSEwork is significantly higher than those with no childhood SHSEhome. The smoking behavior of father and sibling(s) at home could have established social norms by signaling that smoking and exposing others to SHS is acceptable16. It has been posited that social norms are one of the important processes through which one’s environment can affect behaviours22. Within Asian households23, fathers are, generally, in a position of authority, and siblings could be viewed as both family members and peers to the individual8,24. Their collective behaviors at home could enhance the prominence of the normative behaviour25 of smoking in the presence of others. When such behaviors are more commonly observed, individuals could be more susceptible to other factors that also affect tobacco-related health behaviors.
Efforts to promote smoke-free homes by focusing on the household level have been proven to be effective in lowering SHSE in children26. Given the potential impact of various sources of smokers during childhood on tobacco-related behavior and health outcomes in adulthood, efforts to alleviate SHSEhome should take the family context into consideration, ensuring the involvement of family members who are daily smokers at home. This is particularly pertinent during one’s childhood, as children typically have limited power to change the behavior of adults they are living with.
In contrast to findings in childhood SHSEhome, the association of current SHSEhome was positive and significant. This could suggest current norms in the home environment is spread to the workplace or vice-versa27, given that SHSEhome and SHSEwork are happening at the same period. The prevailing social and environmental norms are likely acting on both the home and workplace setting28,29, hence smoke-free policies have the potential to enhance changes in social norms surrounding tobacco-related behavior at the broader, community level30. When the current daily smokers at home include the child identity, the odds of current SHSEwork are elevated more than for the subgroups that include the other current sources only. Prior evidence has shown that parents of smokers tend to have non-negative attitudes towards smoking31,32.
Overall, this study implies that different smoker sources at different phases of an individual’s life may have an impact on accepting, and hence reporting SHSEwork. We examined different sources at different temporal settings, reflecting the changing life-course of the participant. Although we can distinguish between the specific parent who smoked daily at home during childhood, we are unable to do so for current SHSEhome, as they are grouped with the in-laws in the survey. The changing impact of family dynamics33 on SHSEhome as one ages could be further studied using qualitative methods.
Limitations
Our study has limitations. As it is cross-sectional in nature, we cannot establish the causal relationship between current exposure to SHS at home and work. Use of self-reported SHSE is susceptible to social desirability bias and recall bias. Our data captured SHSEhome only from those living in the same household, hence we cannot account for other modes of SHSEhome, such as drifting SHS from neighboring apartments. This would be pertinent in high-density apartment dwellings common in Singapore, which are at higher risk to SHSEhome due to drifting smoke from neighbours34. SHSEhome may have been exacerbated by the COVID-19 pandemic, as many were working and learning from their homes at the time of the study. Drifting SHS from neighboring apartments could be explored in future studies.
Implications
Limitations notwithstanding, our results, taken together with existing studies, demonstrate the importance of reducing SHSEhome in both temporal settings. Specifically, public health policies should target creating smoke-free home environments for children, who are not in the position to influence the actions of their parents or older siblings30, thus lowering the likelihood of childhood SHSEhome and the children commencing smoking in the future16. Community level interventions, especially those focusing on shifting existing social norms on tobacco-related health behaviors, have been found to lead to household and individual level changes30. For example, implementing smoke-free regulations at the workplace is found to be associated with more homes also becoming smoke-free11,35. However, such efforts should consider local contexts36.
CONCLUSIONS
In general, our study found positive associations between SHSEhome and SHSEwork, with the sources of daily smokers at home playing an important role among working adults who are healthy, never smokers, in Singapore. Current SHSEhome is a risk factor for current SHSEwork and the subgroup with the highest risk consists of individuals who are currently living with their children who smoke daily at home. Childhood SHSEhome may have an impact on current SHSEwork, particularly among individuals who lived with their fathers and siblings who smoked daily at home, during their childhood. These results provide additional evidence on the importance of living in a smoke-free home environment because it reduces exposure to SHS at work. Deformalizing smoking in the presence of others at home, in different temporal phases of an individual’s life-course, could lead to meaningful changes in the individual’s exposure to SHS at work.