Recent manuscripts
Archive
Editorial Board
Aims and Scope
Open Access
Indexing
Contact us
Authorship & COI
Principles of Transparency Checklist
Publication Ethics
Crossmark
Data Policies
Supporting Diversity
Instructions to authors (PDF)
Manuscript Types
Manuscript Formatting
How to submit
Special Publications & Reprints
Preprints
Modeling smoking and depression comorbidity in the U.S
1
University of Michigan, Health Management and Policy, United States of America
2
University of Bristol, United Kingdom
3
University of Michigan, Epidemiology, United States of America
Publication date: 2018-03-01
Tob. Induc. Dis. 2018;16(Suppl 1):A369
KEYWORDS
TOPICS
ABSTRACT
Background:
Evidence shows that the relationship between depression and smoking may be bi-directional, with smoking increasing the risk for subsequent depression, and vice versa—translating into significantly higher smoking rates among those with depression compared to the general population. Computational models can be used to assess trends in smoking but have not been utilized to examine populations with behavioral health comorbidities. We develop the first joint model of smoking and depression, projecting future smoking patterns under a 'status quo' scenario.
Methods:
We use a compartmental model to simulate individuals transitioning across smoking and depressive states from birth to age 99 or death. The model is calibrated to reproduce smoking and depression data from the 2005-2014 U.S. National Survey on Drug Use and Health. Current smokers report smoking within the past year and smoked at least 100 cigarettes in their lifetime while those with depression report a major depressive episode in the past year. Parameters for the effects of smoking and depression on each other were drawn from existing literature.
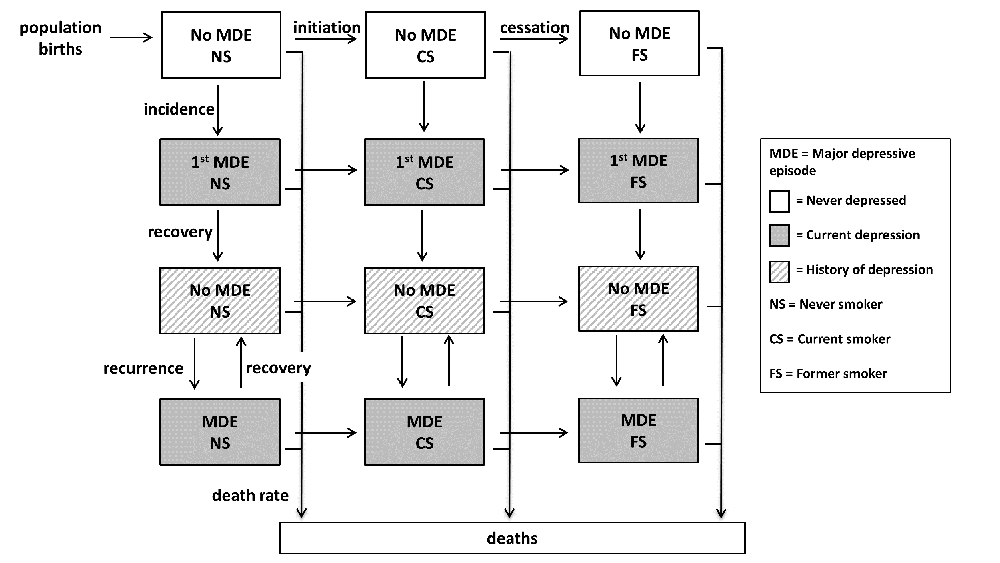
[Smoking and depression model diagram]
Results:
From 2015 to 2050, smoking prevalence among women with depression is projected to decline by 43.5% (27.6% to 15.6%), compared to 46.9% (17.9% to 9.5%) for women who report never having had a depressive episode. Among men with depression, smoking prevalence is expected to decline by 32.0% (34.4% to 23.4%), compared to 39.0% (24.1% to 14.7%) for men who report never being depressed. The likelihood of smoking among those with depression is projected to increase.
Conclusions:
This model can be used to examine trends and identify optimal interventions to address smoking disparities by depressive status. Smoking prevalence among people with depression is expected to decline, though not as rapidly as for those without depression. In the absence of population-level strategies, smoking and tobacco-related diseases will continue to further disproportionately burden people with depression.
Evidence shows that the relationship between depression and smoking may be bi-directional, with smoking increasing the risk for subsequent depression, and vice versa—translating into significantly higher smoking rates among those with depression compared to the general population. Computational models can be used to assess trends in smoking but have not been utilized to examine populations with behavioral health comorbidities. We develop the first joint model of smoking and depression, projecting future smoking patterns under a 'status quo' scenario.
Methods:
We use a compartmental model to simulate individuals transitioning across smoking and depressive states from birth to age 99 or death. The model is calibrated to reproduce smoking and depression data from the 2005-2014 U.S. National Survey on Drug Use and Health. Current smokers report smoking within the past year and smoked at least 100 cigarettes in their lifetime while those with depression report a major depressive episode in the past year. Parameters for the effects of smoking and depression on each other were drawn from existing literature.
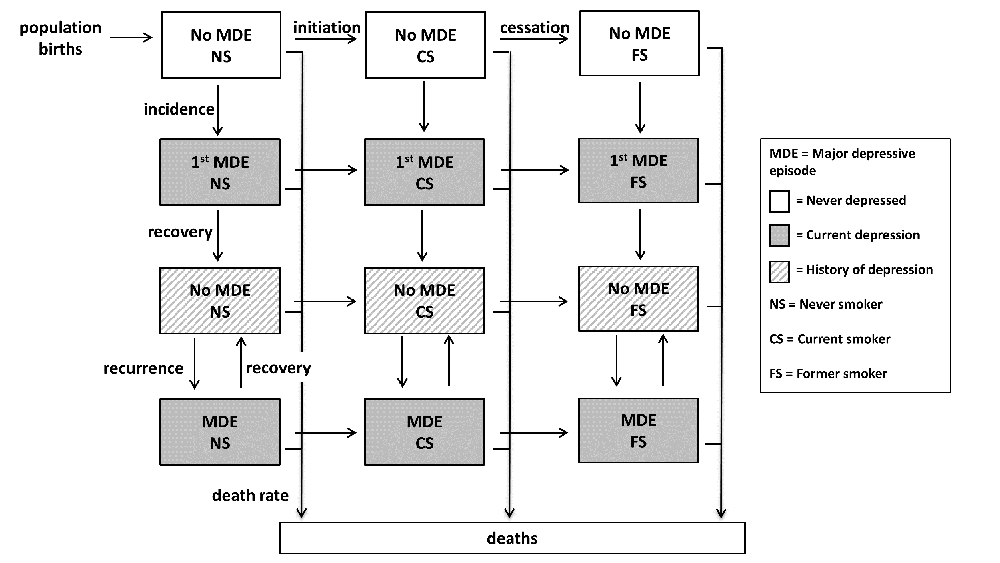
[Smoking and depression model diagram]
Results:
From 2015 to 2050, smoking prevalence among women with depression is projected to decline by 43.5% (27.6% to 15.6%), compared to 46.9% (17.9% to 9.5%) for women who report never having had a depressive episode. Among men with depression, smoking prevalence is expected to decline by 32.0% (34.4% to 23.4%), compared to 39.0% (24.1% to 14.7%) for men who report never being depressed. The likelihood of smoking among those with depression is projected to increase.
Conclusions:
This model can be used to examine trends and identify optimal interventions to address smoking disparities by depressive status. Smoking prevalence among people with depression is expected to decline, though not as rapidly as for those without depression. In the absence of population-level strategies, smoking and tobacco-related diseases will continue to further disproportionately burden people with depression.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.

